Revive Stronger
Glucose Disposal Agents: A Thorough Review of the Evidence
Glucose Disposal Agents (GDAs) have made a quick rise in fitness and are likely promoted by many of your favourite people. When you consume carbohydrates, there is a natural rise in blood glucose levels. There is an upper limit to how much your body wants to allow blood glucose concentrations to rise, this is done to prevent a condition called hyperglycemia. One of the most powerful tools your body has in order to prevent this is a hormone called insulin – a hormone that causes glucose to be shuttled into cells so that it can be removed from the bloodstream. Glucose enters cells through GLUT transporters, think of this like a doorman that holds the door open for glucose and allows it to enter cells.
Some GLUT transporters such as GLUT 1, GLUT 2, GLUT3 and GLUT5 can act independently of insulin; meaning they don’t need insulin to shuttle glucose into the cells. GLUT4 is an insulin-dependant transporter and is the main glucose transporter in skeletal muscle, where most of the body’s glycogen is stored.
Table of Contents
The Claims & The Evidence
GDAs claim to be able to enhance the utilization of blood glucose. They claim to be able to cause glucose to be preferentially shuttled to muscles instead of fat tissue or other sites. Essentially, they claim that they will improve “nutrient partitioning”, meaning that the nutrients consumed will be used to fuel muscle growth and recovery rather than contributing to fat mass.
Proponents of GDAs claim that these are useful supplements in hypercaloric phases (or bulking, massing, gaining, etc.), as they will allow you to use the caloric surplus to gain muscle and not gain fat. GDA supplements are not one ingredient, they are a combination of ingredients put into a supplement. This article will review the literature on the most common ingredients in GDAs, this will include: berberine, cinnamon extract, chromium, alpha lipoic acid and banaba leaf extract
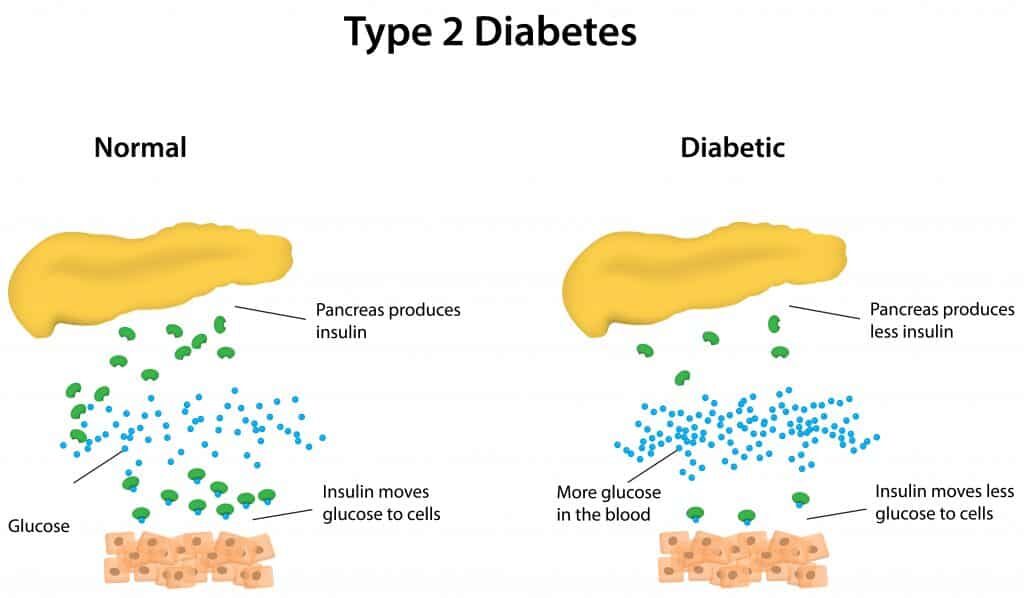
Type II Diabetes – The Basics
Type II Diabetes is a very complicated disease, but I will break it down so that you can understand that data on diabetics cannot be translated to non-diabetic, healthy, active athletes. Pancreatic beta cells secrete insulin in response to high blood glucose levels. Insulin causes glucose from the blood to be stored in tissues throughout the body. Chronically high blood glucose levels, typically in overweight and sedentary individuals, causes constant secretion of insulin to dispose of the glucose. Eventually, pancreatic beta cells cannot keep up with the demand of chronic insulin production and become dysfunctional. Once this happens, insulin secretion is highly diminished, causing blood glucose levels to remain chronically high since they cannot be shuttled through the insulin-dependent GLUT4 transporters.
When blood glucose is chronically elevated, a protein called haemoglobin is covalently bound to glucose, which is a process called glycation. Once haemoglobin is glycated, it is referred to as HbA1C. Haemoglobin is actually part of red blood cells, which have a lifespan of approximately 120 days. Thus, measuring HbA1C gives an accurate idea of glycemic status for the past 2-3 weeks. Remember this, as I will be discussing HbA1C frequently in this article.
In healthy people: blood glucose levels are tightly regulated by functional pancreatic beta-cells that are able to secrete adequate amounts of insulin when needed. When blood glucose goes up, insulin is secreted and glucose is shuttled to adequate tissues – this process does not need external aid in healthy individuals. In people with diabetes, on the other hand, external aid (drugs, supplements, etc.) are needed to shuttle the blood glucose to tissues since insulin is not being secreted to do its job.
Shuttling Glucose Into Muscle
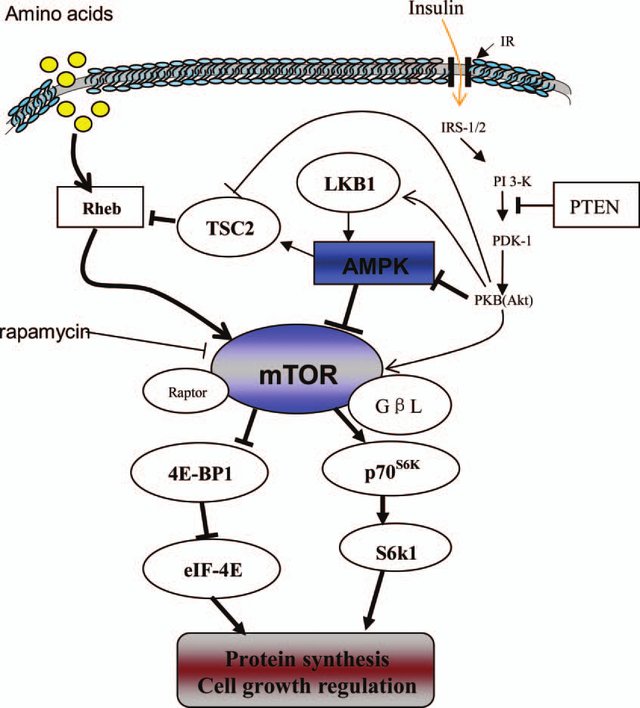
In people with diabetes, the low levels of insulin prevent efficient transportation of glucose into muscle cells via GLUT4 transporters, since they are insulin-dependent. As discussed above, GLUT4 transporters are found in skeletal muscle. One way that glucose can be shuttled into cells via GLUT4 transporters is by activation of AMPK. However, in healthy individuals, insulin will be naturally secreted due to high blood glucose levels and transportation through GLUT4 will occur.
Targeting AMPK activation seems to be a viable method to reduce blood glucose levels in diabetics and is a main mechanism of action of Metformin, a powerful drug typically given to diabetics (Coughlan et al., 2014). AMPK is an energy-sensing protein kinase, specifically, it senses low-energy availability. In periods of low energy, mostly sensed by a high AMP:ATP ratio, AMPK will be activated to conserve energy and will help to shuttle glucose into cells to replenish lost energy. Many GDAs (berberine, cinnamon extract, chromium etc.) exert their main action by activation of AMPK.
Before we jump up in glee, let’s talk about muscle protein synthesis (MPS). The master-regulator of MPS in the body is a protein called mTOR, which is actually directly inhibited by AMPK. High levels of AMPK inhibit MPS likely because MPS is a highly energy-demanding process (Mounier et al., 2011).
Berberine
Perhaps the most common ingredient in GDAs, berberine is a chemical that is extracted from natural sources such as barberry, goldenseal, goldthread, Oregon grape, Phellodendron, and tree turmeric. Berberine is put into GDA products since it has been found to have beneficial effects on glucose metabolism for diabetics but this does not translate to healthy individuals with normal glucose metabolism. Further, much of the literature has been done on mice and cannot be directly applied to humans. Let’s review the literature on berberine, just so you will see what I mean.
A meta-analysis of 27 studies by Lan et al. (2015) compared the effects of:
- Berberine versus placebo
- Lifestyle intervention + berberine versus only lifestyle intervention
- Berberine versus hypoglycemic or lipid-lowering drugs
These were compared in patients with Type 2 Diabetes or hypertension. Berberine intake ranged from 0.6-2.7g/d. They found that berberine was more effective at reducing blood glucose levels, blood pressure, blood lipids than placebo or lifestyle intervention alone and has effects comparable to some drugs.
As previously discussed, in people with Type 2 Diabetes, insulin is not being secreted adequately to dispose of excessive blood glucose. So, how exactly does berberine cause blood glucose to be shuttled into cells?
The main mechanism through which berberine works is by activation of AMPK (Wang et al., 2017). As previously discussed, activation of AMPK will directly inhibit muscle protein synthesis by downregulation mTOR.
A search of the literature revealed no studies on berberine in healthy individuals that were not diabetic, pre-diabetic, dyslipidemic, had Metabolic Syndrome or had other clinical issues that could affect blood glucose. Thus, we cannot make assumptions about how berberine is going to affect the glucose metabolism of a healthy, active adult with normal glucose metabolism. Further, the mechanism of action of berberine is by activation of AMPK, which directly interferes with muscle protein synthesis (Wang et al., 2017; Cheng et al., 2006; Lee et al., 2006). Many people take GDAs after their training, with their highest carb meal to “shuttle nutrients to the right place”… this is probably not the best of ideas if they’re directly activating AMPK
Berberine: No solid data on healthy adults and might interfere with muscle gain.
Cinnamon Extract
Cinnamon extract has been proposed to help with glucose tolerance by AMPK activation, allowing glucose to enter skeletal muscle through GLUT4 transporters (Medagama, 2015). Again, AMPK directly inhibits mTOR, the master regulator of muscle protein synthesis. Keep in mind that we’re talking about cinnamon extract; this is concentrated cinnamon that you would get in pill or concentrated powder form. You probably need a ridiculously high level of regular ground cinnamon bark to actually have measurable effects on muscle.
Further, cinnamon extract seems to be able to delay gastric-emptying, reducing the glycemic response to a meal. However, fibre does the same by increase food viscosity and so does dietary fat by the release of hormones CCK and GLP-1.
Apart from mechanistic data, let’s see what cinnamon extract (both Cinnamomum cassia and Cinnamomum zeylanicum) has shown in human trials.
A meta-analysis by Akilen et al. (2012) looked at the effects of cinnamon on people with Type 2 Diabetes in randomized controlled trials (RCTs). It was found that 1-6g of cinnamon was effective at reducing fasting blood glucose (-0.84mmol/L) and HbA1C (-0.09%) compared to placebo. A previous meta-analysis by Allen et al. (2011), also done in people with Type 2 Diabetes, showed that cinnamon was effective at reducing fasting blood glucose level (-24.59mg/dL) but not at reducing HbA1C. But we need to take this research with a big grain of salt, as you will learn below.
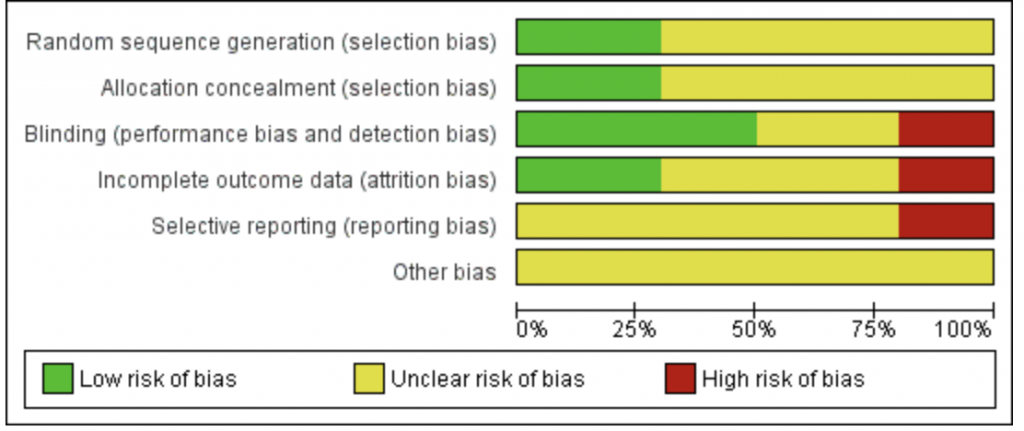
Cochrane Reviews are one of the gold standards in research. The Cochrane Collaboration is a non-profit organization that produces very thorough, unbiased research reviews and meta-analysis on various medical topics. A Cochrane Review was done on the effects of cinnamon on blood glucose (Leach and Kumar, 2011). The Cochrane Review included 10 studies, most of the studies were also included in the meta-analysis by Akilen et al. and Allen et al. It was found that 5 out of the 10 studies showed a high risk of bias, 3 studies showed an unclear risk of bias and only 2 studies had a low risk of bias.
They found that the effects of cinnamon on fasting blood glucose level was inconclusive. Further, there were no differences in HbA1C, serum insulin or post-meal glucose between placebo and cinnamon. Thus, it seems like the research on cinnamon is inconclusive and likely does not favour cinnamon as an effective way to regulate blood glucose.
Similar to berberine, there are no studies looking at the effects of cinnamon on glucose tolerance in healthy, non-diabetic, non-dyslipidemic, active adults.
Cinnamon: The research on glucose tolerance is inconclusive.
At best, it may be beneficial in people with Type 2 Diabetes. If it does have an effect, it’s likely that its through AMPK activation, which would have inhibitory effects on muscle protein synthesis.
*Please do not misinterpret this information. This does not mean that putting cinnamon on your post-workout oatmeal will reduce muscle growth – you would probably need a ridiculously large amount over long periods of time. However, it could mean that taking concentrated cinnamon extract pills post-workout might not be the best of ideas.
Chromium
Chromium can be found in supplements in many forms, but mainly as chromium chelate and chromium picolinate. Their main mechanism of action is through a protein called chromodulin, which acts to augment the signal of insulin in insulin receptors when in the presence of insulin. Further, it also activates AMPK in muscle cells (Zhao et al., 2009). Once again, the actions of AMPK downregulate mTOR, the master regulator of protein synthesis.
A meta-analysis by Suksomboon et al. (2014) looked at the effects of chromium supplementation in people with Type 1 and Type 2 Diabetes. The meta-analysis found that chromium picolinate was effective at reducing fasting blood glucose and HbA1C in diabetics.
Fortunately, there are studies done on chromium supplementation on non-diabetics. One study by Iqbal et al. in 2009 involved 63 participants who were given either chromium picolinate or placebo. These participants were given 1000mcgs of chromium picolinate or placebo. This dose is commonly found in supplements, or even less. After 16 weeks, it was found that chromium supplementation did not improve any measures of glucose metabolism; this includes fasting glucose, HbA1C, insulin sensitivity and glucose effectiveness.
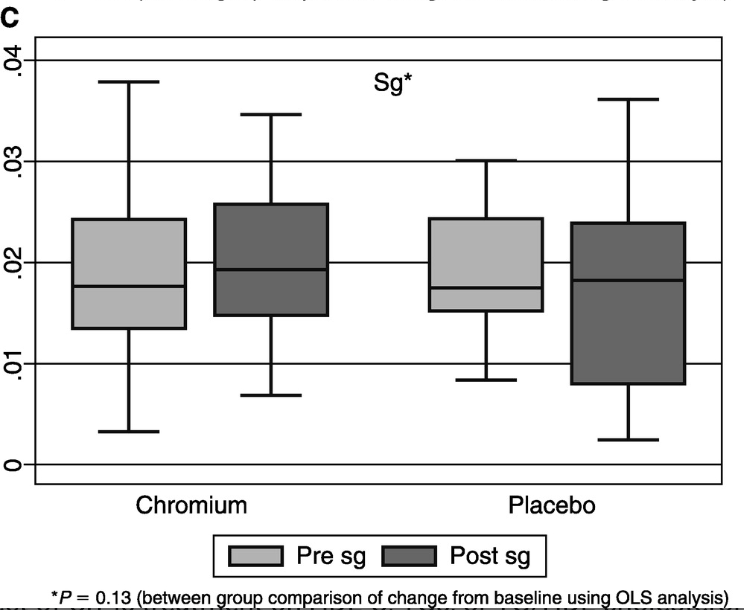
A study by Joseph et al. (1999) looked at the effects that a 12-week resistance training program had with and without chromium supplementation. It was found that following a resistance training program decreased insulin response to glucose and plasma insulin levels by improving insulin clearance. However, chromium supplementation did not result in any further benefits in glucose metabolism. Additionally, a Cochrane Review by Tian et al. (2013) found there was no conclusive beneficial outcomes to chromium supplementation in regards to fasting blood glucose. Further, it found that there is no conclusive and reliable data to show that chromium results in beneficial weight-loss outcomes such as BMI, waist circumference and body fat percentage
Chromium: No effects in healthy individuals in regards to glucose tolerance, weight-loss or resistance training.
Might be beneficial for people with diabetes.
Alpha Lipoic Acid (ALA)
ALA is a naturally occurring amino acid that can be found in various meats, animal products and even some vegetables. ALA has been studied for both its antioxidant and blood-glucose lowering effects. ALA has been shown to reduce Reactive Oxygen Species and Oxidative Stress in rats, thereby enhancing insulin sensitivity in a chronically inflamed state (Henriksen, 2006; Maddux et al., 2001). However, the research on humans is scarce, especially when sufficient antioxidants and other anti-inflammatory agents are consumed as part of a regular diet.
The “NATHAN1” Trial by Ziegler et al. (2011) observed the effects of 600mg of ALA supplementation compared to placebo over 4 years and included 460 diabetic participants. This large study measured HbA1C and other markers of diabetic complications such as Neuropathy Impairment Score. It was found that after 4 years, there was no difference in HbA1C between the ALA and placebo groups.
A study by McNeilly et al. (2011) tested the effects of 1 gram of ALA daily in people with Type 2 Diabetes with and without an exercise protocol. This study split people into two groups that did a 12-week exercise protocol where they went on the treadmill for 30mins at 65% of VO2 max, 5 days per week. After 12-weeks, one group kept performing the exercise protocol and began taking 1g ALA daily while the other group stopped exercising and began taking 1g of ALA daily. There was no difference seen between baseline and post-intervention levels of blood glucose or HbA1C in either group.
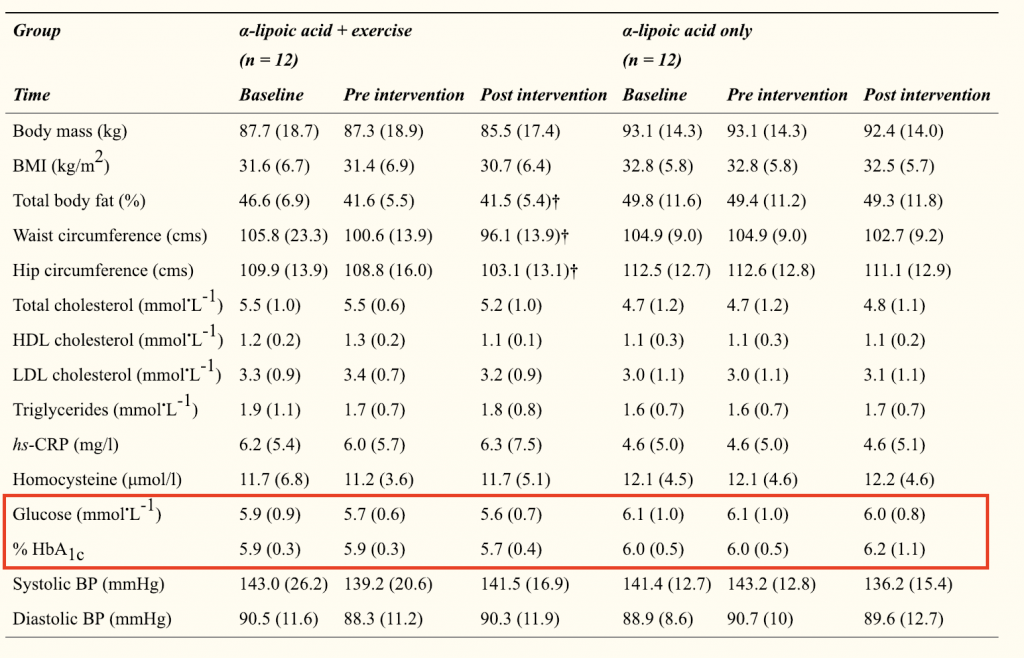
Xiao et al. (2011) tested the effects of 1,800mg of ALA compared to placebo in overweight and obese non-diabetic men and women. Since ALA has been proposed to exert glycaemic control by reducing oxidative stress and inflammation, the researchers wanted to test this in overweight subjects with elevated lipid levels. They found ALA did not improve insulin sensitivity in these subjects.
There is no research looking at the effects of ALA supplementation in healthy, active individuals with high-quality diets. The main proposed mechanism of ALA seems to be by reducing oxidative stress and inflammation. Typically, chronic inflammation and oxidative stress stem from high body fat levels and inactivity (Ellulu et al., 2017). However, an active, trained, healthy individual that consumes a high-quality diet with sufficient fibre, antioxidants and essential fatty acids typically won’t have these concerns. Thus, will have adequate glucose uptake without supplementing with ALA.
Alpha-Lipoic Acid: The bulk of the research has been done in diabetics and rats.
Research on humans in scarce, but likely doesn’t benefit healthy, active individuals with high-quality diets.
Banaba Leaf Extract
Banaba (Lagerstroemia speciosa), otherwise known as Pride of India, is mainly included in supplements due to its content of Corosolic acid (CRA). It’s proposed that Banaba leaf extract works as an insulin agonist, meaning that it can bind to insulin receptors to exert similar actions.
A study that is often referenced to provide “support” for the use of Banaba leaf extract was done by Lieberman et al. (2005). This study was a 12-week intervention where 2 medical doctors and 3 exercise trainers gave a group of 56 subjects thorough nutrition education, 3 cardio + 2 strength sessions per week. They were also given supplements that contained chromium, Gymnema Sylvestre leaf extract, Garcinia cambogia, Bioperine, magnesium, wheat amylase inhibitor, banaba leaf extract, vanadium and bitter melon fruit extract. Thus, on top of being given a nutrition education, training protocol and cardio they were supplemented with 9 ingredients. At the end of 12 weeks, participants lost 13.8lbs (6.9kg)… but let me ask you: do you think was a result of the 16mg of banaba leaf extract or the fact they were working with a full team of experts who taught them how to eat and train for weight loss? I promise you, it was the fact they followed good nutrition and exercise habits.
Another study that is often cited was done by Fukushima et al. (2006); in this study, 31 subjects underwent an Oral Glucose Tolerance Test (OGTT) with 75g of glucose 5-minutes after being given either placebo or 10mg of CRA. This study had a double-blind, placebo-controlled, crossover design meaning that each person received both placebo and the treatment. Blood samples were taken at 30, 60, 90 and 120min after the glucose drink. It was found the CRA group only had lower blood glucose levels after 90 minutes, however, the blood glucose Area Under the Curve (AUC) was not different between groups. Further, the insulin response was lower for the CRA group at 30-min but at no other points. Even though there were points where CRA groups led to lower glucose, the overall response measured by AUC was the same. Additionally, only 4 subjects in this trial had normal blood glucose to begin with, while 19 were diabetic, 7 had impaired blood glucose and 1 had impaired fasting glucose.
A study by Judy et al. (2011) showed that a group of adults with Type 2 Diabetes given a supplement with highly purified CRA were able to reduce blood glucose levels compared to baseline. However, this study was very small; only 5 people per group. Further, it only lasted 15 days and the authors did not measure weight, body composition, calories, macronutrient intake or really anything outside or just blood glucose.
As with the others, there is no research on healthy individuals that are active, trained and have a solid foundation of muscle. However, even in people with diabetes, the evidence does not show conclusive benefits.
Banaba Leaf Extract: No evidence to show that its effective in healthy, active adults without Type 2 Diabetes.
Metformin
Important: Do not take this as medical advice. It is not intended to replace anything said by your physician. If you have been prescribed metformin, speak to your physician and follow what they say.
A recent study has come out that illustrates the effects that Glucose Disposal Agents can have on muscle hypertrophy through the action of AMPK (Walton et al., 2019).
Previous research showed that metformin helped to retain lean muscle mass in a large group of individuals who had either diabetes or impaired fasting glucose levels, but who were not resistance trained or performing resistance training. Unfortunately, this is often used to promote that healthy, resistance-trained individuals could benefit from this effect too.
In the current study, 109 elderly individuals were split into either a metformin (n=54) or placebo group (n=55). The individuals followed a 14-week progressive resistance training protocol that included chest press, lateral pulldown, bicep curls, tricep extensions, squats, leg press and calf press.
At the end of 14-weeks, the placebo group had significantly higher lean body mass compared to baseline (+1.95%, p<0.001), while these changes did not reach significance in the metformin group (+0.41%, p=0.218). Metformin also led to significantly lower gains in thigh muscle area compared to placebo (6.43% vs. 2.27%, p=0.005).
Strength gains tended to be larger in the metformin group, although they did not reach significance. Knee extension 1RM increased by 23.1% in the placebo group and 15.3% in the metformin group (p=0.055). Knee isometric strength increased by 11.8% in the placebo group and 6.7% in the metformin group (p=0.082).
As described above, AMPK is an inhibitor of mTOR, which is the master regulator of protein synthesis. The authors measured the phosphorylation (activation) of basal AMPK in the metformin group compared to placebo. Specifically, they measured the ratio of phosphorylated-AMPK:total-AMPK, which was 21.3% in the metformin group and 1.6% in placebo. However, the between-group differences did not reach significance. A downstream target of AMPK (Phospho-ACC) was found to be significantly higher in the metformin group compared to the placebo group (42.2% vs. 6.2%, p=0.035).
The authors conclude that the significant differences and trends for lower muscle hypertrophy and strength gains in the metformin group compared to placebo were likely due to the activation of AMPK, and its inhibition of mTOR.
While the metformin group still made gains, this study shows how the mechanisms of many GDAs may not be beneficial for muscle hypertrophy or strength for individuals performing resistance training.
Again, if your doctor has prescribed metformin, please do not stop taking it because of this article. This is not intended to be taken as medical advice in any way, shape, or form. Please consult your physician before making any changes to medication protocol
Conclusion
This article has reviewed the literature on berberine, cinnamon, chromium, alpha-lipoic acid and banaba leaf extract.
Berberine shows some effects in people with Type 2 Diabetes through activation of AMPK, but no research in healthy, non-diabetic individuals is seen
Cinnamon extract shows inconclusive research, even in people with Type 2 Diabetes. According to the Cochrane Review by Leach and Kumar (2011), the literature does not show an improvement in fasting blood glucose, HbA1C or weight when supplementing with cinnamon extract.
Chromium didn’t seem to have any effects on healthy individuals in regards to glucose tolerance, weight-loss or resistance training, however, there might be a case for it to be beneficial for people with diabetes.
Alpha Lipoic Acid did not show benefits after 4 years of supplementation in 460 diabetics. Its proposed to aid through antioxidant effects, however, a high-quality diet can provide the necessary antioxidant effects.
Banaba leaf extract: The research has not adequately tested its effects; as it was part of a 12-week protocol with a nutrition and training intervention from a full team of experts. Further, it did not alter the glucose-AUC in response to an OGTT. Lastly, it has not been tested in non-diabetic, healthy trained individuals.
Once again, the literature done on people with diabetes cannot be translated to healthy people without diabetes. In Type 1 Diabetes, pancreatic beta cells are permanently damaged by autoimmune antibodies. In Type 2 Diabetes, pancreatic beta cells become exhausted and cannot exert their functions. In both cases, this results in low insulin secretion and consequently, chronically high blood glucose since it cannot be stored effectively. Thus, in these subjects, supplements may be useful as they don’t have one of the most powerful tools to aid in the shuttling of blood glucose.
As a non-diabetic, when you consume a meal that causes a spike in blood glucose, insulin will naturally be secreted and glucose will be shuttled adequately. Further, since you will likely be in a constant state of recovery from training and replenishing glycogen, your body will be highly receptive to the glucose you are consuming.
As a final point, most of the GDAs discussed in this article function through activation of AMPK, which as I have said repeatedly, inhibits muscle protein synthesis. Therefore, coming home from your workout to have a high dosage of these ingredients with your high-carb meal is probably not a great idea for muscle growth.
The most powerful form of nutrient partitioning comes from being active, performing strenuous exercise regularly and having a solid foundation of muscle mass. Staying relatively lean (<20% body fat for men and <30% in women) is likely beneficial as well, although we’re not sure how higher levels of body fat affect nutrient partitioning in healthy, active and trained individuals. Additionally, having a high-quality diet with sufficient antioxidants is likely beneficial. Once these criteria have been met, then you will likely not be able to further alter nutrient partitioning to favour muscle gain.
References:
Akilen, R., Tsiami, A., Devendra, D., & Robinson, N. (2012). Cinnamon in glycaemic control: Systematic review and meta analysis. Clinical Nutrition (edinburgh, Scotland), 31(5), 609-15. doi:10.1016/j.clnu.2012.04.003
Ashida, H., Furuyashiki, T., Nagayasu, H., Bessho, H., Sakakibara, H., Hashimoto, T., & Kanazawa, K. (2004). Anti-obesity actions of green tea: Possible involvements in modulation of the glucose uptake system and suppression of the adipogenesis-related transcription factors. Biofactors, 22(1-4), 135-140.
Allen, R., Schwartzman, E., Baker, W., Coleman, C., & Phung, O. (2013). Cinnamon use in type 2 diabetes: An updated systematic review and meta-analysis. Annals of Family Medicine, 11(5), 452-9
Cheng, Z., Pang, T., Gu, M., Gao, A., Xie, C., Li, J., . . . Li, J. (2006). Berberine-stimulated glucose uptake in l6 myotubes involves both ampk and p38 mapk. Bba – General Subjects, 1760(11), 1682-1689
Coughlan, K. A., Valentine, R. J., Ruderman, N. B., & Saha, A. K. (2014). AMPK activation: a therapeutic target for type 2 diabetes?. Diabetes, metabolic syndrome and obesity : targets and therapy, 7, 241-53. doi:10.2147/DMSO.S43731
Ellulu, M. S., Patimah, I., Khaza’ai, H., Rahmat, A., & Abed, Y. (2016). Obesity and inflammation: the linking mechanism and the complications. Archives of medical science : AMS, 13(4), 851-863.
Eugester, S.A. (2015). Cinnamon sticks, powder, and dried flowers of the Cinnamomum verum plant. Wikipedia Image. Retrieved January 28th from: https://en.wikipedia.org/wiki/Cinnamon#/media/File:Cinnamomum_verum_spices.jpg
Fukushima, M., Matsuyama, F., Ueda, N., Egawa, K., Takemoto, J., Kajimoto, Y., . . . Seino, Y. (2006). Effect of corosolic acid on postchallenge plasma glucose levels. Diabetes Research and Clinical Practice, 73(2), 174-177
Hattori, K., Sukenobu, N., Sasaki, T., Takasuga, S., Hayashi, T., Kasai, R., Yamasaki, K. & Hazek,i O. (2003). Activation of insulin receptors by lagerstroemin. J Pharmacol Sci. Sep;93(1):69-73.
Henriksen, E. (2006). Exercise training and the antioxidant α-lipoic acid in the treatment of insulin resistance and type 2 diabetes. Free Radical Biology and Medicine, 40(1), 3-12.
Iqbal, N., M.D., M.S.C.E., Cardillo, S., M.D., Volger, S., M.S., R.D., Bloedon, L., M.S., R.D., Anderson, R., Ph.D., Boston, R., M.Sc., Ph.D., & Szapary, P., M.D., M.S.C.E. (2009). Chromium picolinate does not improve key features of metabolic syndrome in obese nondiabetic adults. Metabolic Syndrome and Related Disorders, 7(2), 143-150.
Joseph, L., Farrell, P., Davey, S., Evans, W., & Campbell, W. (1999). Effect of resistance training with or without chromium picolinate supplementation on glucose metabolism in older men and women. Metabolism: Clinical and Experimental, 48(5), 546-53.
Judy, W., Hari, S., Stogsdill, W., Judy, J., Naguib, Y., & Passwater, R. (2003). Antidiabetic activity of a standardized extract (glucosol™) from lagerstroemia speciosa leaves in type ii diabetics :a dose-dependence study. Journal of Ethnopharmacology, 87(1), 115-117
Lan, J., Zhao, Y., Dong, F., Yan, Z., Zheng, W., Fan, J., & Sun, G. (2015). Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension. Journal of Ethnopharmacology, 161, 69-81
Leach, M., & Kumar, S. (2012). Cinnamon for diabetes mellitus. Cochrane Database of Systematic Reviews, 9(9). doi:10.1002/14651858.CD007170.pub2
Lee, Y., Kim, W., Kim, K., Yoon, M., Cho, H., Shen, Y., . . . Kim, J. (2006). Berberine, a natural plant product, activates amp-activated protein kinase with beneficial metabolic effects in diabetic and insulin-resistant states. Diabetes, 55(8), 2256-64.
Lieberman, S., Spahrs, R., Stanton, A., Martinez, L., & Grinder, M. (2005). Weight loss, body measurements, and compliance: A 12 week total lifestyle intervention pilot study. Alternative & Complementary Therapies, 11(6).
Maddux, B., See, W., Lawrence, J., Goldfine, A., Goldfine, I., & Evans, J. (2001). Protection against oxidative stress-induced insulin resistance in rat l6 muscle cells by mircomolar concentrations of alpha-lipoic acid. Diabetes, 50(2), 404-10.
Mayer, M. (2015). Type 2 Diabetes: Metabolomics Reveals Lipid Dysregulation. ThermoFischer.com Retrieved Jan 26th from: https://www.thermofisher.com/blog/proteomics/type-2-diabetes-metabolomics-reveals-lipid-dysregulation/
McNeilly, A. M., Davison, G. W., Murphy, M. H., Nadeem, N., Trinick, T., Duly, E., Novials, A., … McEneny, J. (2011). Effect of α-lipoic acid and exercise training on cardiovascular disease risk in obesity with impaired glucose tolerance. Lipids in health and disease, 10, 217.
Medagama, A. (2015). The glycaemic outcomes of cinnamon, a review of the experimental evidence and clinical trials. Nutrition Journal, 14, 108-108
Mounier, R., Lantier, L., Leclerc, J., Sotiropoulos, A., Foretz, M., & Viollet, B. (2011). Antagonistic control of muscle cell size by ampk and mtorc1. Cell Cycle, 10(16), 2640-2646.
Suksomboon, N., Poolsup, N., & Yuwanakorn, A. (2014). Systematic review and meta-analysis of the efficacy and safety of chromium supplementation in diabetes. Journal of Clinical Pharmacy and Therapeutics, 39(3), 292-306
Tian, H., Guo, X., Wang, X., He, Z., Sun, R., Ge, S., & Zhang, Z. (2013). Chromium picolinate supplementation for overweight or obese adults. Cochrane Database of Systematic Reviews, (20131129).
Wang, H., Zhu, C., Ying, Y., Luo, L., Huang, D., & Luo, Z. (2017). Metformin and berberine, two versatile drugs in treatment of common metabolic diseases. Oncotarget, 9(11), 10135-10146. doi:10.18632/oncotarget.20807
Wu, A. H., Spicer, D., Stanczyk, F. Z., Tseng, C. C., Yang, C. S., & Pike, M. C. (2012). Effect of 2-month controlled green tea intervention on lipoprotein cholesterol, glucose, and hormone levels in healthy postmenopausal women. Cancer prevention research (Philadelphia, Pa.), 5(3), 393-402.
Xiao, C., Giacca, A., & Lewis, G. (2011). Short-term oral α-lipoic acid does not prevent lipid-induced dysregulation of glucose homeostasis in obese and overweight nondiabetic men. American Journal of Physiology: Endocrinology & Metabolism,64(4).
Xu, J., Ji, J., & Yan, X. (2012). Cross-talk between ampk and mtor in regulating energy balance. Critical Reviews in Food Science and Nutrition, 52(5), 373-81
Zhao, P., Wang, J., Ma, H., Xiao, Y., He, L., Tong, C., . . . Li, J. (2009). A newly synthetic chromium complex—chromium ( d-phenylalanine) 3 activates amp-activated protein kinase and stimulates glucose transport. Biochemical Pharmacology, 77(6), 1002-1010
Walton, R., Dungan, C., Long, D., Tuggle, S., Kosmac, K., Peck, B., . . . Peterson, C. (2019). Metformin blunts muscle hypertrophy in response to progressive resistance exercise training in older adults: A randomized, double-blind, placebo-controlled, multicenter trial: The masters trial. Aging Cell, E13039, 13039
We are a personal coaching service that helps you achieve your goals. We want you to become the best version of yourself.



1 thought on “Glucose Disposal Agents: A Thorough Review of the Evidence”
Pingback: Types of Glucose Disposal Agents – Zorayr Manukyan – Zorayr Manukyan
Comments are closed.